Neurologists in Japan have been working overtime recently pursuing cures for the roughly 5,000 people who sustain spinal cord injuries (SCI) every year there.
First, the National Health Ministry approved a breakthrough in regenerative medicine called Stemirac, which uses a special kind of stem cells to help SCI patients regain control of motor skills and bodily functions.
Now, another team of scientists at Keio University in Tokyo — one of the country’s top research institutions — has received authorization for clinical trials using a different type of cell therapy to treat spine injuries.
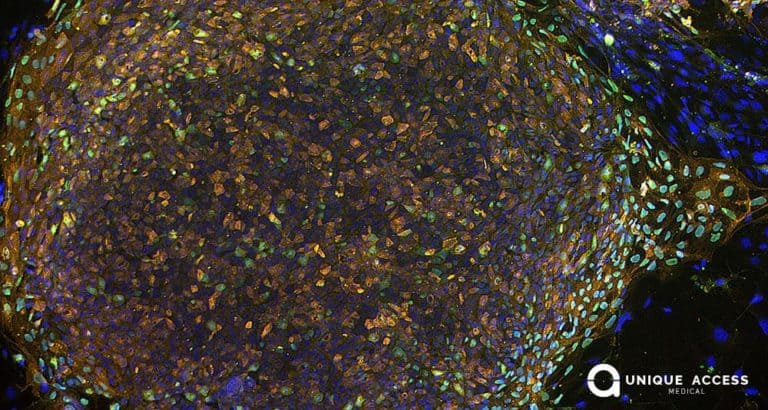
The latest study involves using iPS cells — induced pluripotent stem cells, as they’re known — to create “neural cells” which can enhance the speed at which the brain sends signals and repair damaged spinal tissue. This is only the fifth time iPS cells have been authorized for experimentation by the Japanese health authorities, so researchers are excited by the opportunity.
According to reports out of Keio’s Graduate School of Medicine, the iPS approach has already succeeded in a primate species, as a paralyzed monkey regained the ability to walk after treatment with neural cells. But studying the effects of regenerative medicine on spinal-cord injuries in humans requires the right patients, and indeed a lot of patience.
Even though roughly 100,000 Japanese are living with SCI at any given time, most are considered to be in the “chronic phase” and therefore, until iPS therapy is confirmed 100% safe, they are ineligible for the Keio study. This means patients must be selected from among those 5,000 new SCI cases annually and their results observed for at least one year.
In the meantime, there are already proven forms of regenerative medicine available to treat chronic-phase SCI sufferers from Japan or anywhere else around the world, as well as a groundbreaking surgical procedure known as Epidural Stimulation.
The U.S.Food and Drug Administration and other research organizations in Europe have already approved rigorous clinical testing for targeted spinal-cord neurotechnologies like Epidural Stimulation, but it is only available commercially through Unique Access Medical (UAM).
It has become a leading treatment internationally for all forms of SCI — from significant cervical spine injuries right through the full range of thoracic and lumbar spinal cord injuries, both complete and incomplete, for chronic patients or new ones — and involves surgical implantation of a neurostimulation device that patients can control themselves.
The surgery and an extensive rehabilitation program are performed in our providers’ state-of-the-art facilities in Thailand and India, and are supported by regenerative medicine therapy using allogeneic stem cells.
How long will it be until allogeneic stem cells are complemented by iPS cells as a supportive treatment for spinal-cord injuries? According to Masaya Nakamura, a professor of orthopedics who is leading the Keio University study, his team is aiming to confirm iPS cells’ safety “within two to three years.”
Click here to learn more about UAM’s effective regenerative medicine treatments for paraplegics and quadriplegics, or to speak with one of our patient representatives for a consultation on how UAM can help you improve your condition, contact us today.
Source: Japan Times